Finerenone with empagliflozin beneficial for managing CKD and type 2 diabetes
1. Among patients with both chronic kidney disease (CKD) and type 2 diabetes (T2D) already on a renin-angiotensin system (RAS) inhibitor, a combination of finerenone and empagliflozin resulted in a greater reduction in the urine albumin-to-creatinine ratio (ACR) than either agent alone.
2. Safety profiles for both agents were consistent with existing clinical data, but drug discontinuation was uncommon.
Evidence Rating Level: 1 (Excellent)
Study Rundown: CKD and T2D are common comorbidities and are risk factors for cardiovascular disease and eventual kidney failure. First-line therapies include RAS inhibitors, sodium-glucose cotransporter-2 (SGLT2) inhibitors, finerenone, and glucagon-like peptide-1 receptor agonists. Although there is post-hoc evidence for the additive benefits of simultaneous initiation of SGLT2 inhibitor and finerenone in reducing urine ACR and other clinical outcomes, randomized controlled trial data are lacking. This study sought to investigate this question. Patients with both CKD and T2D, who were already on a RAS inhibitor, were randomized to receive either finerenone, empagliflozin, or their combination. At 180 days, the combination group experienced a greater reduction in urine ACR from baseline than the groups receiving either finerenone or empagliflozin alone. Safety profiles across the groups were as expected, and adverse events resulting in drug discontinuation were uncommon. The trial is limited in its duration and use of a surrogate outcome (urine ACR). Nevertheless, these results, with participants from many countries with a high completion rate, were highly generalizable and supported the simultaneous initiation of empagliflozin and finerenone among patients with CKD and T2D.
Click here to read the study in NEJM
In-Depth [randomized controlled trial]: This study was an international, double-blind, randomized, active-controlled trial to assess the combined initiation of finerenone with empagliflozin against either therapy alone in patients with concurrent CKD and T2D. Patients with diagnosed CKD, an estimated glomerular filtration rate (eGFR) of 30-90 ml/min/1.73m², a urinary ACR of 100-5000mg/g, diagnosed T2D, who had been on a stable, maximally tolerated dose of a RAS inhibitor for ≥1 month, were eligible for inclusion. Exclusion criteria included symptomatic heart failure with reduced ejection fraction, hyperkalemia above 4.8mM, a recent stroke or myocardial infarction, or type 1 diabetes. In total, 800 patients were randomized 1:1:1 to receive either finerenone (10 or 20 mg daily) plus a placebo matching empagliflozin (finerenone group), empagliflozin (10 mg daily) plus a placebo matching finerenone (empagliflozin group), or a combination of both finerenone and empagliflozin (combination group). The primary outcome was to measure the relative change in the log-transformed mean urinary albumin-to-creatinine ratio from baseline to day 180. At day 180, the reduction in urine ACR the combination group 29% greater than that in the finerenone group (least-squares mean ratio of difference in change from baseline 0.71, 95% confidence interval [CI] 0.61-0.82, p<0.001) and 32% greater than the empagliflozin group (least-squares mean ratio of difference in change from baseline 0.68, 95% CI 0.59-0.79, p<0.001). Significantly more participants on combination therapy achieved a UACR reduction of >30% (70.0%), >40% (64.2%), and >50% (54.6%) compared to the monotherapy groups. No unexpected adverse events were reported across the groups, including transient hyperkalemia and eGFR decline. These results demonstrated that for patients with CKD with albuminuria and T2D, initial combination therapy with finerenone and empagliflozin resulted in a greater reduction in urine ACR at 180 days than either drug used alone, with no significant safety concerns.
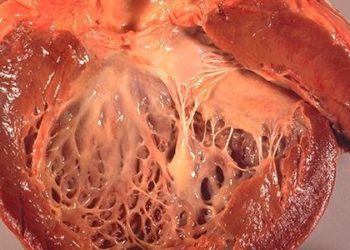
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.