Intraosseous drug administration does not improve survival in out of hospital cardiac arrest
1. In this randomized trial, intraosseous-first vascular access did not result in higher 30-day survival than intravenous-first strategies in adults with out-of-hospital cardiac arrests that required drug therapy.
2. Neurological outcomes did not differ between groups and the percentage of patients with return of spontaneous circulation appeared to be lower among the intraosseous group than the intravenous group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Studies have suggested that the effectiveness of medications used in out-of-hospital cardiac arrests is highly time-dependent. Specifically, this suggests that earlier medication administration may improve clinical outcomes. Various factors may impact the ability to secure intravenous access to such medications. Previous studies have suggested that intraosseous routes may facilitate more rapid drug administration than the standard intravenous route. Currently, international resuscitation guidelines recommend peripheral intravenous access as the primary vascular route. However, there has been ongoing uncertainty about the effectiveness of alternative routes of drug administration in adults with cardiac arrest. This randomized trial aimed to assess the clinical effectiveness of an intraosseous-first strategy in comparison to an intravenous-first strategy in adults with out-of-hospital cardiac arrest. Patients who met inclusion criteria were randomly assigned to receive treatment from paramedics by either an intraosseous-first or intravenous-first vascular access strategy. The primary outcome of this study was survival at 30 days. Secondary outcomes included the return of spontaneous circulation and neurological function at discharge. Results from this study found that the intraosseous-first vascular access strategy did not result in higher 30-day survival than the intravenous-first strategy. Limitations of this study included the small sample size and the lack of collected information regarding resuscitation quality.
Click here to read the study in NEJM
In-Depth [randomized controlled trial]: This randomized trial assessed the clinical effectiveness of an intraosseous-first strategy as compared to an intravenous-first strategy in adults with out-of-hospital cardiac arrest. Adult patients who had an out-of-hospital cardiac arrest and required vascular access for drug administration during ongoing CPR were eligible for this study. Patients were excluded if they had a known or apparent pregnancy. A total of 6,082 patients were randomly assigned to receive treatment from paramedics by either an intraosseous-first (n=3,040) or intravenous-first (n=3,042) vascular access strategy. The primary outcome for this study was 30-day survival, with secondary outcomes including return of spontaneous circulation and favorable neurological function at hospital discharge. At 30 days, 137 of 3030 patients (4.5%) in the intraosseous group and 155 of the 3034 (5.1%) in the intravenous group were alive (adjusted odds ratio, 0.94; 95% confidence interval [CI], 0.68 to 1.32; P=0.74). A favorable neurological outcome was seen at discharge in 80 of 2994 patients (2.7%) in the intraosseous group and 85 of 2986 (2.8%) in the intravenous group (adjusted odds ratio, 0.91; 95% CI, 0.57 to 1.47). Return of spontaneous circulation at any time was observed in 1092 of 3031 patients (36%) in the intraosseous group and 1186 of 3035 patients (39.1%) in the intravenous group (adjusted odds ratio, 0.86; 95% CI, 0.76 to 0.97). Overall, results from this study found that intraosseous-first vascular access did not result in significantly higher 30-day survival than an intravenous-first strategy in adults with out-of-hospital cardiac arrest. Furthermore, there was no apparent difference in the percentage of patients who showed favorable neurological outcomes at hospital discharge. Lastly, the percentage of patients who had a return of spontaneous circulation at any time appeared to be lower among the patients in the intraosseous group than those in the intravenous group.
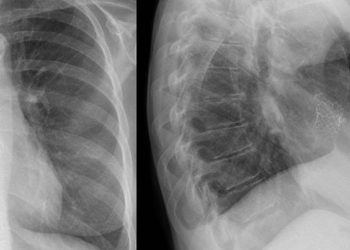
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.