No difference in clinical outcomes between joint replacement and fusion surgeries for ankle osteoarthritis
1. In patients with end-stage ankle osteoarthritis, no differences were seen in outcomes between total ankle replacement (TAR) and ankle fusion (AF) surgeries.
2. There were no significant differences in the rate of adverse events in patients who received TAR as compared to AF surgeries.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Surgical procedures are indicated for patients with severe ankle osteoarthritis that have failed six months of nonoperative management. TAR and AF are the main surgical treatments for ankle osteoarthritis. The present randomized control trial is the first to compare the clinical effectiveness and rate of adverse events between TAR and AF for patients with end-stage ankle osteoarthritis. Patients were followed for one year after surgery. TAR and AF were compared based on the primary outcome of the 52-week change in the Manchester-Oxford Foot Questionnaire walking/standing (MOXFQ-W/S) domain score and the secondary outcomes of 26- and 52-week changes in MOXFQ-W/S, activities of daily living, and quality of life. While both TAR and AF patients had improved MOXFQ-W/S-measured clinical outcomes, there were no significant differences in the magnitude of improvement between groups. There was a greater improvement in activities of daily living, measured by Foot and Ankle Ability Measure-Activities of Daily Living (FAAM-ADL), in the TAR group compared to the AF group. There were no significant differences in the overall rate of adverse events between groups. As a limitation, long-term outcomes could not be evaluated, as the observation period was only 52 weeks. The type of TAR (mobile or fixed bearing) or AF (open or arthroscopic) was not specified, which may introduce unintended heterogeneity in treatment groups.
Click to read the study in AIM
In-Depth [randomized controlled trial]: In this randomized controlled trial, the clinical outcomes and safety of TAR and AF were compared in patients aged 50 to 85 years with end-stage ankle osteoarthritis (n=303). Patients were randomized in a 1:1 ratio to receive TAR (n=152) or AF (n=151) treatment and were followed for 52 weeks. Patient outcomes were measured preoperatively and at 26- and 52 weeks post-operation using MOXFQ-W/S, MOXFQ pain and social interaction domains, and FAAM-ADL. For the primary outcome of the MOXFQ-W/S score, the TAR and AF groups improved by an average of 49.9 and 44.4 points, respectively, from baseline to postoperative 52 weeks. This change was not significantly different between groups. For the secondary outcome, the TAR group demonstrated greater 52-week improvements in the FAAM-ADL scores compared to the AF group (Difference, 6.16; 95% Confidence Interval [CI], 1.54 to 10.78). In terms of safety, 27 (18%) and 36 (24%) of patients in the TAR and AF groups, respectively, experienced at least one serious adverse event, while 82 (54%) and 80 (53%), respectively, experienced at least one adverse event. Wound healing complications (13% and 6% in the TAR and AF groups, respectively) and nerve injuries (4% and <1%, respectively) were more common in the TAR group. Thromboembolic events were less common in the TAR group than in the AF group (3% and 5%, respectively). This is the first study to evaluate the clinical outcomes and safety of TAR and AF and could inform patients and physicians in their clinical decision-making.
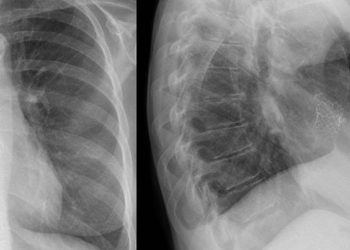
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.