The ACCORD trial: Intensive glucose control associated with increased mortality [Classics Series]
1. Previous studies suggest that intensive blood glucose control reduces the risk of microvascular complications, though questions remained regarding the impact on macrovascular complications and mortality.
2. This study found that targeting HbA1c <6.0% resulted in higher risk of cardiovascular and all-cause mortality as compared with standard therapy (i.e., targeting HbA1c between 7.0-7.9%).
Original Date of Publication: June 12, 2008
Study Rundown: The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial sought to explore whether more intensive glucose control regimens were associated with better outcomes in patients with type 2 diabetes mellitus. Prior to the ACCORD trial, several randomized controlled trials had been conducted regarding blood sugar control in type 2 diabetics. The University Group Diabetes Program (UGDP) study, a randomized controlled trial conducted in 1970, suggested that there was no benefit of glycemic control in new-onset type 2 diabetics. Subsequently, a second randomized trial conducted in Japan demonstrated a reduction in the incidence of microvascular complications with better blood sugar control, while a third demonstrated no significant reduction in cardiovascular events in patients with better blood sugar control. Perhaps the most notable study, however, was the UK Prospective Diabetes Study (UKPDS), a randomized, controlled trial involving 5,102 patients with newly diagnosed type 2 diabetes. The study was conducted over a 20 year period (1977-1997) and conclusively demonstrated that microvascular complications could be reduced by intensively controlling blood glucose.
Despite all these studies, however, there was no sufficiently powered, randomized trial explicitly examining the effect of intensive glucose control on cardiovascular outcomes. Thus, the aim of the ACCORD trial was to determine whether intensive therapy to control blood glucose levels (targeting HbA1c <6.0%) in type 2 diabetics would reduce cardiovascular events, compared to standard therapy (targeting HbA1c from 7.0-7.9%). In summary, this trial demonstrates that intensive glucose lowering significantly increases the risk of cardiovascular (HR 1.35; 95%CI 1.04-1.76) and all-cause mortality (HR 1.22; 95%CI 1.01-1.46) as compared with standard therapy.
Click to read the study in NEJM
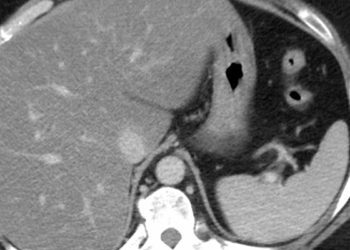
In-Depth [randomized, controlled study]: Originally published in 2008, this study was conducted in 77 centres across Canada and the United States. Patients were eligible for the trial if they had type 2 diabetes and an HbA1c≥7.5%. Moreover, eligible patients were either between 40-79 years of age with cardiovascular disease or 55-79 years of age with anatomical evidence of atherosclerosis, albuminuria, left ventricular hypertrophy, or ≥2 additional risk factors for cardiovascular disease (i.e., dyslipidemia, hypertension, current smoker, or obesity). Patients were randomized into two different treatment arms: 1) intensive therapy targeting HbA1c<6.0% or 2) standard therapy targeting HbA1c between 7.0-7.9%. The primary outcome was nonfatal myocardial infarction (MI), nonfatal stroke, or death from cardiovascular causes. Secondary outcomes included all-cause mortality.
A total of 10,251 participants were involved in the final analyses. There was no significant difference in the composite primary outcome between the study groups (HR 0.90; 95%CI 0.78-1.04), though the intensive group experienced significantly fewer nonfatal MIs (HR 0.76; 95%CI 0.62-0.92) and significantly more deaths from cardiovascular causes (HR 1.35; 95%CI 1.04-1.76). It was also found that all-cause mortality was significantly higher in the intensive group (HR 1.22; 95%CI 1.01-1.46). Notably, there were significantly more instances of hypoglycaemia in the intensive therapy group as compared with standard therapy (16.2% vs. 5.1%, p<0.001).
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.