The CAPRICORN trial: Beta-blockers in acute myocardial infarction [Classics Series]
Image: PD
1. Carvedilol significantly reduced mortality from cardiovascular causes and recurrent non-fatal MI.
2. While carvedilol treatment was associated with a 23% relative risk reduction in all-cause mortality, this did not reach statistical significance.
3. These findings are consistent with previous trials exploring the benefits of beta-blockers in managing acute MI.
Original Date of Publication: May 5, 2001
Study Rundown: The CAPRICORN trial demonstrated that beta-blockers confer considerable benefits in patients suffering from acute myocardial infarction (MI). While carvedilol was associated with a relative risk reduction in all-cause mortality of 23%, this did not reach statistical significance because the alpha for this endpoint was re-adjusted to 0.005 partway through the study. Carvedilol did, however, significantly decrease mortality from cardiovascular causes and recurrent non-fatal MI. While previous studies examined beta-blockade prior to the widespread use of reperfusion and ACE inhibitors in managing MIs, the findings from the CAPRICORN trial are consistent with the older data.
Please click to read study in The Lancet
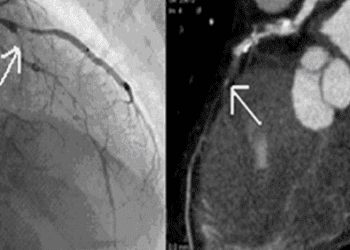
In-Depth [randomized, controlled study]: While previous studies had established the benefits of beta-blockade in managing MI, these trials were conducted prior to widespread use of thrombolysis or angioplasty for reperfusion, and also prior to the introduction of angiotensin-converting-enzyme (ACE) inhibitors. Thus, the CAPRICORN trial, originally published in 2001 in The Lancet, was conducted to explore the long-term efficacy of carvedilol in patients suffering from acute MI, taking into account recent advances in management. Patients were included if they were 18 years of age, had suffered a definite MI 3-21 days before randomization, had a left ventricular ejection fraction (LVEF) <40%, and had concurrent treatment with ACE inhibitors for at least 48 hours, unless there was a proven intolerance to ACE inhibitors. They were randomized to either the carvedilol group (maximum dose of 25 mg PO BID) or to placebo. The co-primary endpoints were 1) all-cause mortality and 2) all-cause mortality and cardiovascular hospital admissions. Secondary endpoints were sudden death and hospital admission for heart failure, while other endpoints were recurrent non-fatal MI and all-cause mortality or recurrent non-fatal MI.
A total of 1,959 patients were recruited from 163 centres in 17 different countries, and they were followed for a mean of 1.3 years. Approximately 46% of patients required reperfusion therapy, largely through thrombolysis, though some did undergo primary angioplasty. Notably, about 98% of patients were being treated with ACE inhibitors at the time of randomization. While all-cause mortality was reduced by 23% in the carvedilol group, this did not reach statistical significance. There were also no significant differences between the two groups in terms of secondary endpoints. Patients in the carvedilol group, however, did experience significantly lower rates of cardiovascular-caused mortality and non-fatal MI.
By Aimee Li, M.D.; Andrew Cheung, M.D.
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT. Content is produced in accordance with fair use copyrights solely and strictly for the purpose of teaching, news and criticism. No benefit, monetary or otherwise, is realized by any participants or the owner of this domain.