Vena caval filters in pulmonary embolism prophylaxis [Classics Series]
Image: PD
1. Permanent vena caval filter placement in addition to anticoagulant therapy helps prevent short-term occurrence of pulmonary embolism but increases the risk of recurrent DVT in the long-term
2. There is no significant difference in efficacy between LMWH and UFH during early anticoagulant therapy for PE prophylaxis
Original Date of Publication: February 1998
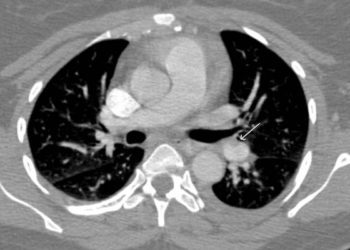
Study Rundown: In patients who are at high-risk for pulmonary embolism (PE) and have a contraindication to anticoagulation, an vena caval filter is a potential option to reduce the risk of PE. This multicenter, randomized study in France is the only randomized, controlled trial that has sought to determine whether filter placement decreases the incidence of PE, as well as deep vein thromboses (DVT) both in short-term and long-term follow-up. The study demonstrated that the use of a permanent vena caval filter in addition to heparin therapy reduced the occurrence of a PE in the short-term (OR 0.22; 95%CI 0.05-0.90). The data, however, also showed that in long-term follow-up of two years, there was a significant increase in recurrent DVTs in patients who received a filter (OR 1.87; 95%CI 1.10-3.20). This most likely relates to thrombosis at the filter site, but it may counteract the benefits gained earlier with the reduction in PE occurrence.
In summary, this study showed that filters lower the risk of PE in the short-term, but later increase the risk of recurrent DVT. It also confirmed the results of previous studies that showed no difference in effectiveness between low molecular-weight heparin (LMWH) and unfractionated heparin (UFH) for early anticoagulant therapy. Overall, the evidence in this study does not support the use of IVC filters in addition to anticoagulant therapy to prevent PE’s and recurrent DVT’s. Interestingly, this study excluded patients with DVT who had a contraindication to anticoagulation, which is one of the commonly cited indications for filter placement.
Click to read the study in NEJM
In-Depth [randomized, controlled study]: This study was a multicenter, non-blinded, 2×2, randomized-controlled trial that randomized 400 patients to vena caval filter placement or no placement, and to receive LMWH or UFH as a bridge to warfarin. Patients over 18 years of age with confirmed DVT with or without concomitant symptomatic pulmonary embolism, and whose physicians believed they were at high risk for a PE, were eligible for the study. Patients with history of IVC filter placement, contraindication to anticoagulant therapy, or likelihood of non-compliance were excluded. Two hundred patients were assigned to receive vena caval filters. One hundred ninety-five of the 400 total were assigned to LMWH while the other 205 were assigned to UFH for the first 8-12 days of anticoagulant therapy. The subjects underwent a baseline V/Q scan and/or pulmonary angiography to evaluate for a PE. All subjects were transitioned to warfarin therapy after 8-12 days for a duration of 3 months or maintained on UFH if oral anticoagulation was not possible. Patients were followed for 2 years. The primary outcome was occurrence of a PE within the first 12 days of anticoagulant therapy. The secondary outcome was occurrence of PE, DVT, major filter complication, and/or major bleeding during the follow-up period.
Filter vs. No Filter
The study demonstrated that there were significantly fewer patients (2 vs. 9 patients) in the filter group compared to the non-filter group who had had a pulmonary embolism in the first 12 days of anticoagulation therapy (OR 0.22; 95%CI 0.05-0.90). Results were similar when analysis was adjusted for heparin therapy and presence of PE at enrollment. In the 2-year follow-up, there was a significantly higher number of recurrent DVTs in the filter group compared to the no-filter group (OR 1.87; 95%CI 1.10-3.20). There was no significant difference in PE incidence, mortality, or major bleeding between the two groups at the 2-year mark.
LMWH vs. UFH
There was no significant difference in incidence of PE’s or DVTs between the two anticoagulant groups during the first 12 days as well as the 2-year mark. There was also no statistical significance in mortality or adverse effects between the two groups.
There was no evidence of statistically significant interaction between filter and heparin anticoagulant therapy for both primary and secondary outcome events.
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.