2 Minute Medicine Rewind July 19, 2021
1. In a large trial, a multi-component interventional program did not reduce antimicrobial use amongst people with advanced dementia living in nursing homes.
Evidence Rating Level: 1 (Excellent)
Antimicrobials are commonly prescribed to individuals within nursing homes, often without sufficient evidence of infection, thus failing to acknowledge the goals of care of patients. This clustered randomized clinical trial sought to evaluate a multi-component intervention to improve management of suspected infections by consulting best practices from both infectious disease and palliative care. 426 participants were divided into two groups, an intervention group with 227 patients (mean [SD] age, 85.3 [8.6] years; 83.7% women) and a control group with 199 patients (mean [SD] age, 87.7 [8.0] years 81.9% women). Facilities in the intervention group received a multicomponent training program including seminars, an online course, management algorithms, and feedback forms. The primary outcome measured was the number of antimicrobial courses for suspected urinary tract infections (UTI) or lower respiratory infections (LRI). For the duration of the study (12 months), 27.1% and 33.9% of patients in the intervention group and control group, respectively, received at least 1 course of antimicrobial treatment. Although the adjusted marginal rate of antimicrobial courses was 33% lower in the intervention arm, the difference was not statistically significant. The secondary outcomes were the number of antimicrobial courses for UTI or LRI when minimal criteria for initiation was absent and the number of burdensome procedures performed to evaluate patients with suspected UTI or LRI. There was no statistically significant difference in the secondary outcomes between the two groups. Therefore, future research is needed to establish better antimicrobial prescribing practices for people with advanced dementia.
1. In a large cohort from Sweden, six variables focused on symptoms, observations, and mode of arrival to the hospital, were found to be predictive of 7-day and 30-day mortality in septic patients.
Evidence Rating Level: 3 (Average)
Sepsis is associated with substantial morbidity and mortality worldwide. There are various scoring tools to predict sepsis mortality in the emergency department. However, these tools are based off vital signs and do not include patient presentation characteristics. This cross-sectional study sought to identify such variables predictive of 7-day and 30-day mortality amongst septic patients in the emergency department. The study included 445 septic patients (median age, 73 years; 52.6% men). It found that the six most important variables of predicting 7-day mortality in descending order were fever, abnormal verbal response, low oxygen saturation, arrival by emergency medical services, abnormal behaviour or level of consciousness, and chills. The study demonstrated that these six variables had a sensitivity of 0.84 (CI 95%, 0.78–0.89), specificity of 0.67 (CI 95%, 0.64–0.70), positive predictive value of 0.31 (CI 95%, 0.28–0.33) and negative predictive value of 0.96 (CI 95%, 0.95–0.97), collectively. For 30-day mortality, the six most important predictors in descending order were abnormal verbal response, fever, chills, arrival by emergency medical services, low oxygen saturation, and breathing difficulties. These variables demonstrated a sensitivity of 0.87 (CI 95%, 0.81–0.93), specificity of 0.64 (CI 95%, 0.61–0.67), positive predictive value of 0.41 (CI 95%, 0.39–0.44) and negative predictive value of 0.95 (CI 95%, 0.92–0.97). Overall, the study concluded that such variables would be important to include in future prediction tools of mortality amongst septic patients. However, these results need to be further validated in other cohorts to evaluate their generalizability.
1. In a cohort of extremely premature infants, high screen time contributes to adverse cognitive, executive function, and behavioural outcomes at ages 6 to 7.
Evidence Rating Level: 2 (Good)
Increased screen time is known to be negatively associated with cognitive development and executive function. Similarly, children who are born extremely premature, less than 28 weeks’ gestation, have been shown to be at increased risk of behavioural problems and executive function deficits. However, there is limited research on association of screen time with adverse outcomes in the high-risk preterm population. This cohort study sought to address this gap in literature, and included 414 participants (ages 6 to 7; 55% male), from which 238 had high screen time (>2 hours screen time) and 176 had low screen time (<2 hours screen time). The primary outcome measured was association of screen time with cognition, language, executive function, and behaviour at an early school age for children who were born extremely premature. It demonstrated that children with high screen time had decreased full scale intelligence quotient scores after adjustment of various confounding variables (mean [SE] difference, −3.92 [1.64]; P = 0.02). They also have significantly higher mean scores on the Behavior Rating Inventory of Executive Function metacognition index (mean [SE] difference, 2.82 [1.34]; P = 0.04) and on the global executive composite percentiles (mean [SE] difference, 7.49 [2.99]; P = 0.01).The secondary outcomes assessed were the association between high screen time and rates of structured physical activity, rates of overweight (defined as body mass index ≥85th percentile), and rates of obesity (defined as body mass index ≥95th percentile). Children high screen time were more likely to have lower mean [SD] minutes per day of structured physical activity than children with low screen time (8.07 [12] vs 4.42 [9]; P < .001). They also had higher rates of overweight (62 [28%] children; P < .001) and obesity (33 [15%] children; P < .001). Therefore, this is one of the first studies to demonstrate adverse associations of high screen time in children who were extremely premature, highlighting importance of educating patients and parents on these risks.
1. In a large cohort of hospitalized patients in Maryland, it was found that Black patients with aortic stenosis had a lower incidence of surgical treatment when compared to their White counterparts.
Evidence Rating Level: 2 (Good)
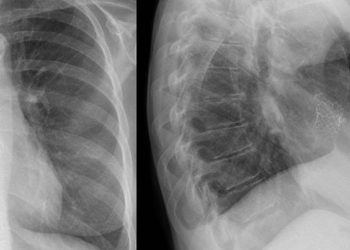
Aortic stenosis is one of the most common valvular heart diseases which is managed through a surgical aortic valve replacement (SAVR) or a transcatheter aortic valve replacement (TAVR). Racial inequities have been recognized in cardiology interventions such as these however the extent of this problem has not been investigated. This retrospective cohort study aims to assess the extent of racial/ethnic inequities in aortic stenosis, SAVR, and TAVR. The study cohort consisted of 433,078 hospitalized patients in Maryland, from which 14,336 patients had aortic stenosis and 418,742 did not have aortic stenosis. It found that among hospitalized patients in Maryland, Black and Hispanic patients had a lower incidence of any inpatient diagnosis of aortic stenosis (IRR, 0.45; 95% CI, 0.42–0.49; P<0.001 for Black versus White; and IRR, 0.67; 95% CI, 0.58–0.78; P<0.001 for Hispanic versus White). Among patients with an inpatient diagnosis of aortic stenosis, Black patients had a significantly decreased incidence of SAVR when compared to White patients (1934 versus 2916; IRR, 0.66; 95% CI, 0.55–0.79; P<0.001) and Hispanic patients (1934 versus 4036; IRR, 2.09; 95% CI, 1.31–3.21; P=0.002). Similarly, among patients in an inpatient diagnosis of aortic stenosis, Black patients had a statistically significant decreased incidence of TAVR when compared to White patients (2513 versus 3805; IRR, 0.66; 95% CI, 0.56–0.77; P<0.001). Hispanic patients admitted with aortic stenosis had an incidence of TAVR of 3553, however, there was no statistically significant difference when compared to White or Black patients. The study concluded that there are racial inequities in the surgical treatment of aortic stenosis. However, further research is needed to further elucidate the causes of such inequities so that systemic changes can be implemented in an effort to reduce the disparities.
1. In a cohort of thyroid cancer patients, multidisciplinary tumor boards were associated with changes in their management plan and improved clinician knowledge.
Evidence Rating Level: 2 (Good)
Multidisciplinary Tumor Boards (MDT), consisting of several healthcare specialists, are frequently used in medicine when managing patients with various cancers. They have been shown to significantly influence treatment plans for patients, increase patient and physician satisfaction, and may also improve survival. Although thyroid cancer is quite prevalent worldwide, there is limited research to establish guidelines for management, and thus, it would benefit from MDT. This study aimed to assess an Endocrine MDT for alterations in management on thyroid cancer cases based on its recommendations. The study included 286 presentations of thyroid carcinoma, 70% of which were women and 6.7% of which were pediatric cases. The primary outcome measured was the incidence of change in management after presentation of the case at MDT. It was found that management chance was recommended in 49 (15%) of MDT presentation, with the most common alteration being request for additional imaging (42.5%). Secondary outcomes measured were patient characteristics associated with higher likelihood of change in management, evaluation of the frequency of various types of change in management, attendee perception of the usefulness of MDT, and any changes in their clinical practice because of MDT. There were no significant associations between management plan changes and patient characteristics. The study evaluated 91 evaluations of the MDT from attendees. 54 attendees (59.3%) indicated regular attendance in the MDT meetings and 99% of attendees indicated improvement in their patient care and teaching due to the MDT. Additionally, 28.9% of attendees indicated management changes learned from the MDT and 21% indicated changes in their planned imaging work-up. Therefore, the study is one of the first to conclude that MDT presentations led to higher rate of management changes in thyroid cancer patients and were associated with increased evidence-based practices among clinicians.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.