2 Minute Medicine Rewind July 27, 2020
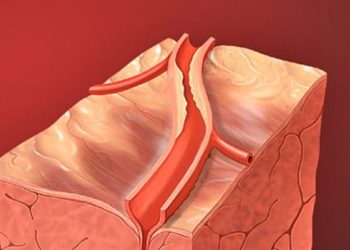
Prior tonsillectomy is associated with an increased risk of esophageal adenocarcinoma
1. Having a prior tonsillectomy was correlated to a greater risk of developing esophageal adenocarcinoma, with an odds ratio of 1.7.
Evidence Rating Level: 2 (Good)
Esophageal adenocarcinoma (EAC) is a subtype of esophageal cancer that has gradually grown in incidence over the years, increasing six-fold in the United States between 1975 and 2001. Currently, Barrett’s Esophagus (BE) is the sole known lesion to be a precursor for EAC, and factors such as for obesity, use of tobacco, and gastroesophageal reflux disease (GERD) have been identified as associated risk factors. Currently however, the association between tonsillectomy and development of EAC is not well characterized, despite these procedures being relatively common and previously associated with greater risk for several diseases, including deep neck malignancy and infection. To analyze whether prior tonsillectomy was an independent risk factor for development of EAC, this retrospective cohort study examined the association between tonsillectomies and EAC or BE with high grade dysplasia (HGD). The study involved examining the records of 452 patients who underwent an esophagectomy procedure for EAC/HGD. The control group was 1102 patients who underwent a thoracic surgery not related to EAC/HGD. 19.9% of EAC/HGD patients had a prior tonsillectomy, whereas 12.7% of control patients had a prior tonsillectomy (p=0.0003). Patients who previously underwent a tonsillectomy were more likely to have EAC/HGD than those who did not (OR 1.7, 95% CI: 1.3-2.3). This association was still present after adjusting for covariates such as obesity, tobacco use, GERD history, male gender, and white race (OR 1.8, 95% CI: 1.2-2.7). A proposed biological mechanism is that removing the tonsils dampens the immune response by lowering IgA levels, so that when pathogens are encountered, cytokine production increases and chronic inflammation ensues, leading to EAC. As a retrospective cohort study, causality cannot be inferred from this study alone, and as such, further investigations are warranted to further characterize the mechanisms by which tonsillectomy may be associated with EAC development. Nonetheless, study findings reveal a possible novel independent risk factor for EAC development which may be used to inform clinical decision making in the future.
1. Cardiometabolic risk factors are unchanged in a 12-month randomized controlled trial examining sugar-sweetened, artificially sweetened, and unsweetened beverages.
2. Sweet preference is decreased most after switching from sugar-sweetened to unsweetened beverages.
Evidence Rating Level: 1 (Excellent)
Consuming sugar-sweetened beverages (SSBs) has long been associated with negative health outcomes, such as obesity, Type II diabetes mellitus, and cardiovascular disease. However, there have been mixed results in associating artificially sweetened beverages (ASBs) to these outcomes. A particular concern is that consuming ASBs may contribute to a stronger preference for consuming sugary foods. Reducing refined sugar consumption is correlated with lower ratios of serum triglyceride to high-density lipoprotein cholesterol (TG:HDL-C). Low TG:HDL-C also predicts cardiometabolic outcomes such as insulin resistance, coronary atherosclerosis, and myocardial infarction. In this randomized controlled trial aimed, researchers sought to determine the effect of SSB, ASB, and USB consumption on TG:HDL-C, body weight, and sweet preference. Two hundred and three individuals who regularly consumed at least one sugary beverage daily were assigned to either have free SSBs, ASBs, or USBs delivered to their homes for 12 months, and asked to consume these beverages at the same frequency as they previously did with sugary beverages. The change in TG:HDL-C was the same among all 3 groups: The adjusted mean change±SE was 3.2±5.7 for SSBs, -2.4±5.4 for ASBs, and -3.2±5.1 for USBs (p = 0.65). Body weight (p = 0.66) and fat mass (p = 0.27) were also the same. However, participants in the highest tertile of trunk fat had a significant body weight increase (p = 0.002) in the SSB group (4.4±1.0 kg) compared to ASB (0.5±0.9 kg) and USB (-0.2±0.9 kg). Finally, sweetness threshold (the concentration rated as being of medium sweetness) was decreased in USBs but unchanged in ASBs (p = 0.0001 and p = 0.02 respectively). Participants’ favourite sugar concentrations were decreased in both USBs and ASBs (-2.3±0.4% m/v, p < 0.0001 and -1.1±0.5% m/v, p = 0.02 respectively). At least on a relatively short term basis of one year, study findings did not provide evidence of SSB substitutes conferring significant health benefits in terms of TG:HDL-C ratio, although both ASBs and USBs were found to lower body weight in individuals with central adiposity. USBs do appear to be the most beneficial substitute of the two however, as they were found to have the most favourable effect on altering sweet taste preference overtime.
1. A vision screening program for kindergarteners in Ontario, Canada diagnosed for the first time 7.2% of all screened children with a visual problem.
Evidence Rating Level: 2 (Good)
In Canada, around 20% of children between 3 and 6 years old have amblyopia or other clinically significant visual problems (such as hyperopia, myopia, and astigmatism). Despite its high prevalence, and eye examinations being covered by health insurance in Ontario, 86% of children younger than 6 have not been screened for visual problems. This is highly problematic, as the Canadian Pediatric Society recommends a minimum of 1 screening between 3 and 5 years of age, since treatments for amblyopia are most effective before 8 years of age. Should these issues be missed, visual disturbances may manifest as difficulties in schooling and infer implications to development longterm. In this prospective cohort study, the feasibility for implementing an early visual screening program in Ontario kindergartens was analyzed as a potential solution to this problem. Screening was conducted at 43 schools for 5884 children in junior kindergarten (age 4) and senior kindergarten (age 5). Those who did not pass the screening test were booked for an examination with an optometrist. The results showed that 68.9% of referred children attended the follow-up appointment, whether this was located at school or at the optometrist’s office. Overall, 10.7% of screened children were diagnosed with a visual problem, and for 67.2% of those diagnosed, it was their first eye examination. As well, 90.4% of the children had positive feelings about the vision games involved in the screening process. Overall, this intervention led to the first diagnosis of 7.2% of all screened children, though further research is needed to increase the rate of referred children attending follow-up examinations. Nonetheless, study findings suggest that in-school vision screening with follow-up eye examinations is an effective strategy for identifying at risk children early on, and may be used as a potential model for other locations. This study led to the implementation of a visual screening program for senior kindergarten students in Ontario.
1. Heritability and shared environmental factors account for BMI variation in sibling pairs during middle childhood, whereas non-shared environmental factors account for variation in adolescence.
Evidence Rating Level: 2 (Good)
In the United States, childhood obesity is a widespread public health problem, estimated to affect 13% of 2-5 year olds and 20.6% of 12-19 year olds, with cases carrying on into adulthood in 90% of teens. The factors that predispose children to obesity can be genetic or environmental. Previous twin and family studies have provided insight on how genetic and environmental factors influence obesity risk: However, they’ve shown mixed results regarding the relative contributions of genetics and environment, and tended to be limited in their generalizability, such as by focusing on a specific age. Therefore, this current study adds on to previous research by implementing an adoption design, examining biological siblings raised together, raised apart, or raised with non-biological siblings. The sample consisted of 897 children taken from the Early Growth and Development Study, and the Early Parenting of Children study. The measures were BMI, home type (adoptive or birth homes), and genetic relatedness among sibling pairs. For environmental factors, a common environment referred to factors shared comparably by all siblings in a household, whereas a unique environment referred to factors that disproportionately affected siblings in a household. The results showed that the factors influencing BMI vary depending on age. In adolescent sibling pairs, home type was the strongest predictor, with those in a birth home having a 14% higher BMI than an adoptive home (p < 0.001). In middle childhood pairs, genetic heritability accounted for 63% of the variation in BMI (SE = 0.11; p = 0.008), common environment accounted for 31% (SE = 0.10; p < 0.001), and a unique environment accounted for 6%. In adolescent pairs and siblings that spanned the two age groups, heritability and common environment influences were not found to contribute significantly to BMI variation, suggesting that unique environmental factors accounted for most of the variation. Through this design, the relative contributions of genetics and environmental factors for child BMI were estimated. These results could have implications for future interventions that target shared environmental factors in a household during middle childhood, to reduce the risk of obesity.
1. The SHISA3 gene was found to be silenced through promoter methylation at higher levels in breast cancer tissues compared to normal breast tissues.
Evidence Rating Level: 1 (Excellent)
Breast cancer (BC) accounts for 15% of tumor related deaths in women, translating to over 627,000 deaths worldwide in 2018 alone. Late diagnosis is considered to be a primary reason for high BC mortality rates, which can be attributed to a scarcity of reliable biomarkers for early stage diagnosis. On the molecular scale, the Wnt signalling pathway plays a role in mammary gland development, with Wnt proteins controlling the growth of ducts in mammary tissue. As well, abnormal activation of this pathway has been correlated to BC development, and so has stabilization of β-Catenin, a regulator of this pathway. SHISA3 is a potential tumour suppressor gene, with the SHISA3 protein acting as an antagonist to Wnt/β-catenin signalling. Epigenetic inactivation of SHISA3 has been found in laryngeal squamous cell and nasopharyngeal carcinoma, though it has not been thoroughly investigated in BC. The current study aimed to investigate SHISA3 gene expression levels in BC cell lines and tissues, as a reduction in SHISA3 expression may provide a biological mechanism for BC development. Three BC cell lines, as well as BC and normal breast tissue samples from 103 patients, were examined in this study. The results found that mRNA levels of SHISA3 were significantly lower in BC tissues than normal breast tissues, as much as 22 times lower in the invasive ductal carcinoma subtype. Additionally, the promoter of SHISA3 was found to be methylated at higher rates in BC tissues than normal tissues (61% vs 18% of samples respectively). Methylation of the promoter was experimentally found to effectively silence the SHISA3 gene. Furthermore, ectopic expression of SHISA3 was shown to substantially reduce the migration ability and proliferative potential of these cells. Study findings appear to identify SHISA3 as a tumour suppressor gene that may have powerful therapeutic implications in BC.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.