2 Minute Medicine Rewind October 2, 2023
Exposure to Neighborhood Walkability and Residential Greenness and Incident Fracture
1. In this longitudinal cohort study, neighborhood walkability and greenness were associated with decreased fracture risk.
Evidence rating level: 2 (Good)
Neighborhood walkability and greenness are associated with health benefits, namely by promoting greater levels of physical activity, reducing exposure to pollution, increasing social connections, and reducing psychological stress. This longitudinal study aimed to examine whether walkability and greenness are associated with fracture risk. 23,940 participants were recruited for this cohort study in Ningbo, China between June 2015 and January 2018. Participant observation continued until February 2023. Mean (SD) age was 63.4 (9.4) years. During the follow-up of 134,638 person-years, 3322 incident fractures occurred. A decrease in fracture risk was associated with every interquartile range (IQR) increment in neighborhood walkability and greenness, with a hazard ratio of 0.88 (95% CI, 0.83-0.92) and 0.84 (95% CI, 0.80-0.89) respectively. Furthermore, for neighborhoods in the highest quartile for walkability, greenness reduced fracture risk with a hazard ratio of 0.62 (95% CI, 0.46-0.82). This cohort study demonstrates that exposure to neighborhood walkability and residential greenness are both associated with decreased fracture risk. A limitation of this study is that the authors did not control for confounding variables other than air pollution. This is important to consider because having a residential address in a walkable neighborhood with more greenspaces may be associated with higher socioeconomic status, which was not accounted for in the current study. Other potential confounders such as smoking, alcohol consumption, and BMI were also not adjusted for. Overall, this study adds to the growing literature suggesting that neighborhood walkability and greenness are important determinants of health.
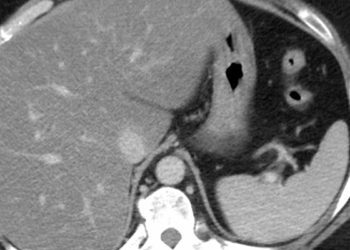
New-Onset Age of Nonalcoholic Fatty Liver Disease and Cancer Risk
1. In this case-control study, younger age of onset of NAFLD was associated with greater cancer risk, with greatest risk for digestive and pulmonary cancers.
Evidence rating level: 3 (Average)
The prevalence of non-alcoholic fatty liver disease (NAFLD) is projected to reach 33.5% of the global population by 2030, as the age of onset becomes increasingly younger. Previous research suggests that NAFLD is associated with a greater risk of liver cancer, GI cancers, and all cancer types. Researchers hypothesized that earlier age of onset of NAFLD would be associated with greater cancer risk. This cohort study was conducted between 2006 and 2021 and included participants from the Kailuan Cohort study. For every identified case of NAFLD, an age and sex-matched control was randomly selected to create the control cohort. There were 31,848 individuals included in both the NAFLD and the control groups. After a median follow-up of 10.16 (95% CI, 7.89-11.67) years, 2415 patients were diagnosed with cancer. Younger age of NAFLD onset was associated with greater cancer risk (ages 45-54 years: average hazard ratio (AHR) 1.50; 95% CI, 1.15-1.97; ages 55-64 years: AHR, 1.13; 95% CI, 0.97-1.33; ages >65 years: AHR, 0.75; 95% CI, 0.45-1.27; p for interaction < .001). Among those who developed NAFLD prior to age 45, the risk of cancer was greatest for digestive AHR 2.00 (95% CI, 1.08-3.47) and lung AHR 2.14 (95% CI, 1.05-4.36) cancers. One limitation of the study is that only 17.2% of participants were female, leading to potential sex bias in the results. Overall, this study demonstrates that developing NAFLD at a younger age increases cancer risk, which may become a more significant global health concern as the prevalence of NAFLD continues to increase worldwide.
1. In this cohort study, uptake of the 2018 European Society of Cardiology Syncope Guidelines by emergency departments was associated with greater diagnostic yield and accuracy.
Evidence rating level: 2 (Good)
Syncope is a common complaint in emergency departments (EDs), accounting for about 1% of all ED visits. Researchers aimed to assess whether the use of the 2018 European Society of Cardiology (ESC) Syncope Guidelines would have an impact on diagnostic accuracy, diagnostic yield, or healthcare costs. This study was conducted across 5 Dutch hospitals. 521 patients who presented to the ED following a syncopal episode were included in this study. The first cohort (October 2017 to September 2019, n = 275) received usual care. The second cohort (October 2017 to September 2019, n = 246) received care after the implementation of ESC Syncope Guidelines. Patients were then seen at a one-year follow-up appointment to evaluate diagnostic accuracy by applying ESC criteria or, if not possible, evaluation by an expert committee. Implementation of the ESC guidelines was associated with greater diagnostic accuracy compared to usual care (86% vs.69%; risk ratio 1.15; 95% CI 1.07 to 1.23) and greater diagnostic yield (89% vs. 76%, 95% CI of difference 6 to 19%). There was no associated change in healthcare costs. On an individual level, implementing ESC guidelines resulted in reduced syncope-related costs for patients (saving €908 per patient; 95% CI €34 to €1782). A limitation of this study is that while the use of ESC guidelines was encouraged in the emergency departments of the intervention group, their use was not enforced, likely resulting in inconsistent use. Overall, this study demonstrates that implementing the use of the ESC Syncope Guidelines in an emergency department is beneficial for improving diagnostic yield and accuracy, as well as reducing the financial burden on patients. Future research may assess whether greater use of these guidelines improves health outcomes for patients, such as reducing the incidence of subsequent syncopal episodes.
1. In this prospective cohort study, the types of carbohydrates consumed were associated with long-term trends in participants’ weight.
Evidence rating level: 2 (Good)
In this prospective cohort study, researchers aimed to examine the association between carbohydrate intake and weight changes over time. 136,432 healthy participants under age 65 were included in this study. Data were collected from the Nurses’ Health Study (1986-2010), Nurses’ Health Study II (1991-2015), and Health Professionals Follow-Up Study (1986-2014). Nutrition data were collected via repeated dietary assessments and validated questionnaires. Participants’ weight was monitored over time, with an overall trend of gaining an average of 1.5 kg every four years, and 8.8 kg over 24 years. Changes in carbohydrate intake were also calculated over time. All analyses were adjusted for many confounding variables, including physical activity, smoking, alcohol consumption, fat intake, and protein intake. Over a 4 year period, a 100 g/day increase in added sugar was associated with an average of 0.9 kgs of greater weight gain, while a 10 g/day increase in fiber intake was associated with an average of 0.8 kg less weight gain. Furthermore, greater carbohydrate intake from whole grains, fruits, and non-starchy vegetables was inversely associated with weight gain, while greater intake of refined grains and starchy vegetables was directly associated with weight gain. These associations were more pronounced for individuals who were overweight or obese compared to those with a normal BMI. The main limitation of this study is that dietary assessments relied on self-reporting. As well, researchers did not adjust for overall caloric intake as a confounding variable. Overall, this study demonstrates that the type of carbohydrates one consumes is an important aspect of weight changes over time. Physicians may use this information when counseling patients on weight, emphasizing the importance of carbohydrate quality for weight control over time.
Five-year results of a treatment program for chronic hepatitis B in Ethiopia
1. In this pilot program conducted in Ethiopia, researchers demonstrated the long-term benefits and feasibility of treatment for chronic hepatitis B (CHB) infections in an under-resourced setting.
Evidence rating level: 2 (Good)
It is estimated that 296 million people worldwide are living with chronic hepatitis B (CHB) infections. Complications from untreated CHB infections include liver cirrhosis, liver failure, and hepatocellular carcinoma (HCC). In sub-Saharan Africa, under 1% of people living with CHB receive treatment. Researchers aimed to determine the feasibility and efficacy of a large-scale CHB treatment program in Africa. This pilot treatment program took place in Addis Ababa, Ethiopia. Adults over age 18 with CHB infection, defined as being seropositive for hepatitis B surface antigen for > 6 months, were recruited for the study in 2015. Of the 1303 patients included in the study, 291 were started on antiviral therapy within the 5-year follow-up period. Treatment eligibility was based on the European Association for the Study of the Liver (EASL) Guidelines, including those with liver cirrhosis, significant liver fibrosis, ALT>80 IU/L with viral load >2000 IU/mL, or family history of HCC in first-degree relatives with viral load >2000 IU/mL. For those receiving treatment, the estimated 5-year HCC-free survival was 99.0% for patients without baseline cirrhosis, compared to 88.8% in patients with compensated cirrhosis, and 54.2% in patients with decompensated cirrhosis (p<0.001). Patients with decompensated cirrhosis at the start of the study had a higher risk of death during the follow-up period with an adjusted hazard ratio (AHR) of 44.6, 95% CI 6.1–328.1, as did those over age 40, AHR 3.7, 95% CI 1.6–8.5. Furthermore, treatment was associated with decreased liver stiffness, with a median change from baseline after 1, 3, and 5 years of treatment of −4.0 kPa,−5.2 kPa, and -5.6 kPa, respectively. This pilot program is evidence of treatment efficacy and feasibility of treating CHB infections in a resource-limited setting. Further work will hopefully include treatment programs for a greater number of people.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.