Convalescent plasma does not improve survival in patients hospitalized with COVID-19
1. A similar proportion of patients died within 28 days of randomization in both groups (high-titre convalescent plasma vs. usual care).
2. Allocation to convalescent plasma had no significant effect on the proportion of patients discharged from hospital within 28 days.
Evidence Rating Level: 1 (Excellent)
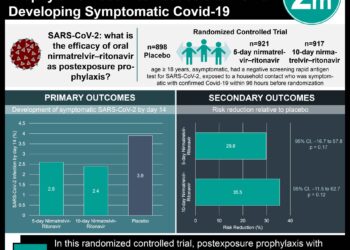
Study Rundown: Convalescent plasma is a form of passive immunotherapy that has been used to treat influenza, pneumonia, and SARS-CoV in the past. While some studies suggest that convalescent plasma may help to reduce mortality in individuals with severe respiratory infection, evidence surrounding this is mixed. This randomized controlled trial aimed to evaluate the efficacy and safety of convalescent plasma therapy in patients hospitalized with COVID-19. Patients in the convalescent group received two units intravenously; one at the time of randomization and the second at least 12 hours after the first dose. The primary outcome was all-cause mortality at 28 days of randomization, while key secondary outcomes included time to discharge from the hospital and receipt of invasive mechanical ventilation or death. According to study results, high-titre convalescent plasma did not improve survival or other prespecified clinical outcomes in COVID-19 patients. This trial was limited by a lack of regular follow-up as outcomes were only assessed at 28 days and 6 months. The study also did not compare the efficacy of convalescent plasma on variants of SARS-CoV-2, such as B.1.1.7 which is predominant UK. Nonetheless, it provided valuable insight into the use of high-titre convalescent plasma for hospitalized patients with COVID-19.
Click to read the study in The Lancet
Relevant Reading: A Randomized Trial of Convalescent Plasma in Covid-19 Severe Pneumonia
In-depth [randomized controlled trial]: Between May 28, 2020, and Jan 15, 2021, 16 287 patients were assessed for eligibility across 177 UK hospitals. Included patients were of any age, with clinically suspected or laboratory confirmed SARS-CoV-2 and no medical history that may put them at significant risk of partaking in the trial. Altogether, 11 558 patients (5795 in the convalescent plasma group and 5763 in the usual care group) were included in the analysis. The mean patient age was 63.5 years (standard deviation [SD] 14.7) and the majority (87%) were receiving oxygen at randomization.
There was no significant difference in the primary outcome of 28-day mortality between the convalescent plasma therapy group (1399 of 5795, 24%) and usual care (1408 of 5763, 24%) group (rate ratio [RR] 1.00, 95% confidence interval [CI] 0.93-1.07, p=0.95). This was also the case when comparing across prespecified patient subgroups (RR 1.00, 95% CI 0.93-1.08, p=0.93 for patients with a positive SARS-CoV-2 test) and those without detectable SARS-CoV-2 antibodies at randomization. The secondary outcome concerning patient discharge from hospital within 28 days was not significantly affected by allocation to convalescent plasma therapy (66% in convalescent plasma group vs. 66% in usual care group, RR 0.99, 95% CI 0.94-1.03, p=0.57). Similarly, among those not receiving mechanical ventilation at randomization, there was no significant difference in the proportion of patients progressing to invasive mechanical ventilation or death (29% in convalescent plasma group vs. 29% in usual care group, RR 0.99, 95% CI 0.93-1.05, p=0.79). Overall, findings from this study show that use of high-titre convalescent plasma does not improve survival or other clinical outcomes in patients hospitalized with COVID-19.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.