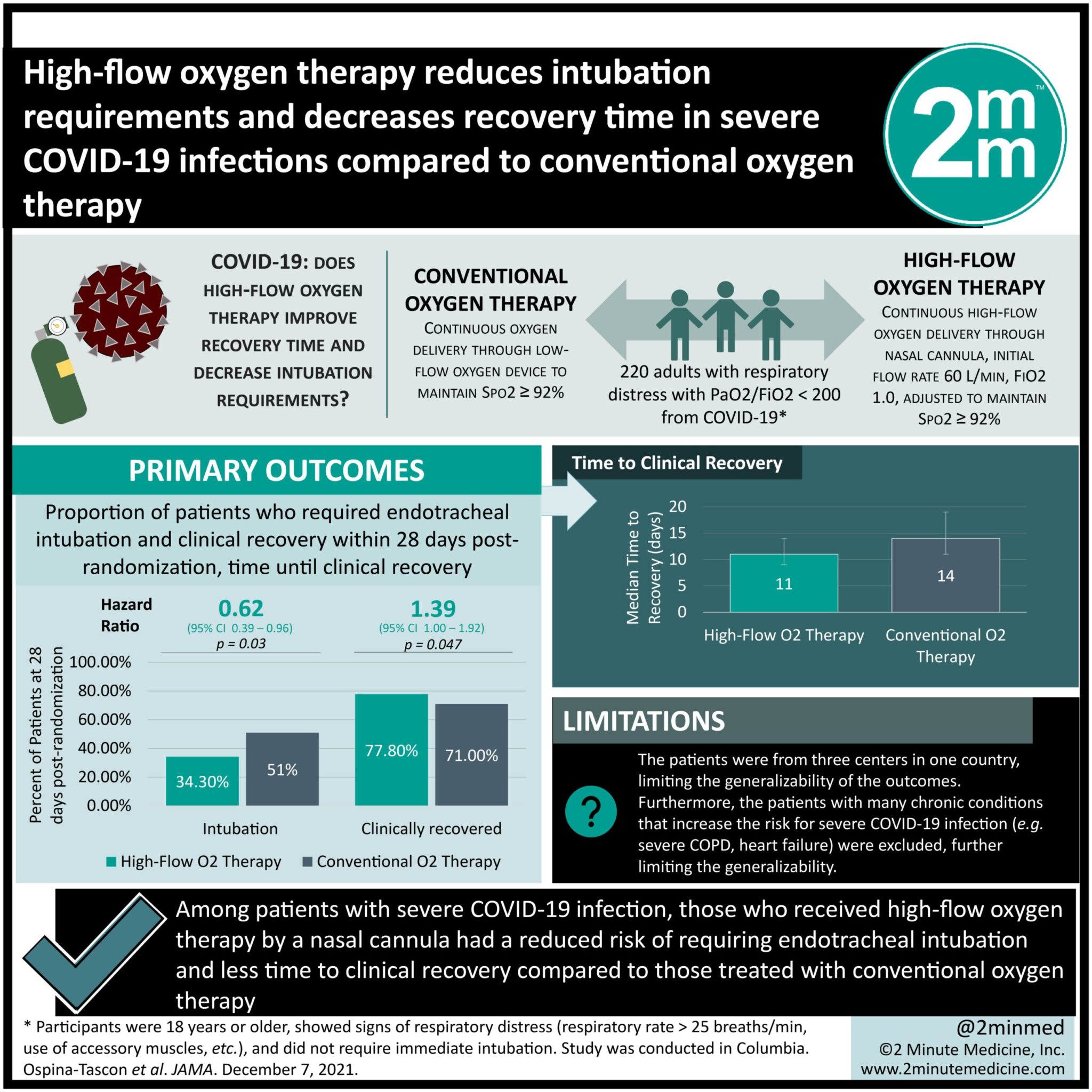
#VisualAbstract: High-flow oxygen therapy reduces intubation requirements and decreases recovery time in severe COVID-19 infections compared to conventional oxygen therapy
1. Among patients with severe COVID-19 infection, those who received high-flow oxygen therapy with a nasal cannula had a reduced risk of requiring endotracheal intubation and less time to clinical recovery compared to those treated with conventional oxygen therapy
Evidence Rating Level: 1 (Excellent)
Study Rundown: Despite the majority of COVID-19 cases resulting in asymptomatic or mild disease, many infected patients progress to acute hypoxemic respiratory failure. Arterial hypoxemia is a common characteristic among severe COVID-19 cases, and its management consists of oxygen supplementation to improve hypoxemia and reduce respiratory efforts. Some data demonstrated that high-flow oxygen therapy might reduce the need for endotracheal intubation. This randomized clinical trial investigated whether high-flow oxygen therapy through a nasal cannula reduces the need for intubation and time to clinical recovery in patients with severe COVID-19 compared to conventional oxygen therapy. This study was conducted in three hospitals in Columbia between August 13, 2020, and January 12, 2021. Adults were included if they had a confirmed SARS-CoV-2 infection, acute respiratory failure with a ratio of partial pressure of arterial oxygen to fraction of inspired oxygen less than 200, signs of respiratory distress, and did not require immediate intubation. Two hundred twenty patients underwent randomization to receive nasal cannula high-flow oxygen therapy (99 participants) or conventional oxygen therapy (100 participants). The co-primary outcomes were the proportion of patients who required endotracheal intubation and time until clinical recovery within 28 days post-randomization. At day 28 post-randomization, 34/99 (34.3%) with high-flow oxygen therapy and 51/100 (51%) with conventional oxygen therapy required intubation (hazard ratio [HR]: 0.62 [95% CI: 0.39-0.96]; p= 0.03). Seventy-seven patients (77.8%) randomized to high-flow oxygen therapy recovered within 28 days compared to 71 patients (71%) randomized to conventional oxygen therapy. Furthermore, the median time to clinical recovery was 11 (IQR: 9-14) days and 14 (IQR: 11-19) days in the high-flow oxygen therapy and conventional oxygen therapy cohorts, respectively. Overall, this study demonstrated that high-flow oxygen therapy with a nasal cannula decreased intubation need and time to recovery in severe COVID-19 infections complicated by acute hypoxemic respiratory failure. Notably, the exclusion criteria included patients with many chronic conditions that increase the risk for severe COVID-19 infection, such as severe COPD and heart failure limiting the generalizability of these findings to this vulnerable population.
Click to read the study in JAMA
Relevant Reading: High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.