2 Minute Medicine Rewind February 6, 2023
1. A randomized trial for a blood pressure (BP) self-management program, involving 6 months of telehealth coaching for hypertensive young adults, found no difference in systolic or diastolic BP at 6 months and 12 months follow-up.
2. There was greater frequency of home BP monitoring in the intervention group at 6 and 12 months, with decreased sodium intake and increased physical activity at 6 months, but not 12 months.
Evidence Rating Level: 1 (Excellent)
An estimated 20-30% of young adults aged 18-39 have hypertension (HTN), with fewer than half of them attaining adequate blood pressure (BP) control. As there are few trials examining interventions for BP self-management in this population, the MyHEART program was created to encourage BP monitoring, promote lifestyle changes, and improve understanding of antihypertensives, amongst young adults with HTN. This current randomized controlled trial compared changes in BP at 6 and 12 months, between young adults enrolled in MyHEART and those undergoing usual care. The study population consisted of adults aged 18-39 years recruited from 2 healthcare authorities in the Midwestern United States, with at least 2 medical office visits coded for HTN. These individuals were randomized 1:1 to care as usual or the 6-month MyHEART program. This program involves evidence-based self-management strategies, such as telehealth coaching with adult education specialists, individualized HTN educational content, and monitoring BP at home. These participants received 20 minute calls every 2 weeks from coaches who had a background in motivational interviewing. In total, there were 316 patients (159 in control and 157 in intervention), with a median (IQR) age of 35 (31-37) years. At baseline, the systolic BP (133.00 [SD 12.67] mmHg for control; 132.59 [11.36] mmHg for intervention) and the diastolic BP (87.04 [81.6] mmHg for control; 86.45 [7.76] mmHg for intervention) were comparable between groups. The study showed that at 6 months and at 12 months, there were no differences in 24-hour ambulatory systolic or diastolic BP between the groups: At 6 months, the systolic BPs were 130.69 [13.99] and 128.14 [11.36] mmHg for control and intervention respectively (p = 0.12), and at 12 months, they were 129.47 [14.71] and 128.54 [11.95] for control and intervention respectively (p = 0.59). However, in both groups, there were significant decreases from baseline in systolic and diastolic BPs at 6 and 12 months. As well, there were significant differences between the groups in monitoring home BP at least once weekly (64% for intervention vs 9.6% for control at 6 months, p < 0.001; 34.9% for intervention vs 8.9% for control at 12 months, p < 0.001). There were also significant differences between groups in sodium intake and physical activity at 6 months, but not at 12 months. Overall, this study showed that the MyHEART program was not associated with differences in BP between control and intervention at 6 and 12 month follow-up, but did demonstrate differences in lifestyle changes, such as home BP monitoring.
1. For patients with a history of lymphoma or breast cancer, anthracycline use is associated with a higher incidence of congestive heart failure (CHF) at 25 years follow-up.
2. Chemotherapy without anthracycline in patients with lymphoma or breast cancer was not associated with higher CHF incidence.
3. Patients receiving a dose of greater than 180 mg/m2 of anthracycline were associated with higher CHF incidence, but not with a dose of less than 180 mg/m2.
Evidence Rating Level: 3 (Average)
Anthracyclines are chemotherapy agents used in lymphoma or breast cancer that have known dose-dependent associations with cardiotoxicity, and in particular, congestive heart failure (CHF). However, the risk factors that mediate this association and the long-term incidence are not well-known. Therefore, this population-based case-control study aimed to compare the incidence of CHF in patients with lymphoma or breast cancer history who did and did not undergo anthracycline therapy, matched by age, sex, and other comorbidities (such as hypertension, coronary artery disease, and obesity) to a control cohort. The study population consisted of patients treated with chemotherapy for lymphoma or breast cancer between 1985 and 2010, matched to control patients in a 1:1.5 ratio. In total, there were 2196 participants, 812 with a cancer history treated with chemotherapy, and 1384 in the control group. The study found that those with a cancer history had a higher risk of developing CHF compared to the control (hazards ratio 3.25, 95% CI 2.11-5.00, p < 0.001). This association remained significant when examining participants with history of anthracycline use (HR 2.56, 95% CI 1.02-6.41, p = 0.04). However, the association was not significant for cancer patients who did not have anthracycline therapy (HR 1.78, 95% CI 0.83-3.81, p = 0.14). In addition, the incidence of CHF amongst those treated with anthracycline was greater than the control group at 1, 5, 10, 15, 20, and 25 years (p < 0.001 for all), while there was no difference in CHF incidence between cancer patients not treated with anthracycline compared to control. There was also a dose-dependent association, with no significant difference in CHF incidence for patients who received less than 180 mg/m2 of anthracycline, but a higher risk for those receiving 180-250 mg/m2 (HR 0.54, 95% CI 0.19-1.51) and greater than 250 mg/m2 (HR 1.23, 95% CI 0.52-2.91). Furthermore, apart from age, no other comorbidities or risk factors were associated with CHF, and there were no differences in CHF incidence for lymphoma versus breast cancer patients. Overall, this study demonstrated that for patients with lymphoma or breast cancer history, anthracycline therapy in doses greater than 180 mg/m2 is associated with a higher incidence of CHF compared to control, whereas chemotherapy without anthracycline is not associated with a higher CHF incidence.
1. Patients with Type 2 Diabetes taking glucagon-like peptide-1 receptor agonists (GLP-1 RAs) have a lower incidence of diabetic retinopathy (DR), compared to those not taking GLP-1 RAs.
2. A Mendelian randomization analysis found that an increase in GLP1R gene expression was associated with decreased risk for background and severe nonproliferative DR subtypes, but not proliferative DR and overall DR.
Evidence Rating Level: 2 (Good)
Diabetic retinopathy (DR) affects greater than 100 million individuals internationally. It can be classified into 3 types (in order of severity): Background DR, severe nonproliferative DR, and proliferative DR. Currently, glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are diabetes medications associated with reductions in cardiovascular morbidity and mortality, as well as stroke. However, they have also been hypothesized to reduce the risk of DR, since the expression of GLP1R, the target of GLP-1 RAs, are prevalent in the retina. The current population matched cohort study based in Sweden examined the incidence of DR amongst patients with diabetes who did and did not use GLP-1 RAs, and also conducted a summary-data-based Mendelian randomization analysis. The cohort consisted of patients diagnosed with Type 2 Diabetes between 2006 and 2015, with each patient using GLP-1 RAs matched to randomly selected patients not using GLP-1 RAs, matched by age, sex, and duration of disease. The Mendelian analysis used single nucleotide polymorphisms (SNPs) associated with GLP1R expression in the pancreas, and correlated that with DR outcomes. In total, there were 14,119 patients included, with 2390 taking GLP-1 RAs and 11,729 patients who did not use GLP-1 RAs. The median (IQR) follow-up time was 2.03 (1.07-3.18) years for those using GLP-1 RAs and 1.92 (0.99-3.47) years for those not using GLP-1 RAs. The study found that the incidence of DR was 5.97 per 1000 person-years for GLP-1 RA users and 12.85 per 1000 person-years for non-users. Therefore, the incidence of DR was significantly lower in GLP-1 RA users (HR 0.43, 95% CI 0.29-0.61, p < 0.0001). Additionally, the Mendelian randomization analysis found that an increase in GLP1R expression by 1 standard deviation was associated with lower background DR risk (OR 0.83, 95% CI 0.71-0.97, p = 0.0162) and severe nonproliferative DR (OR 0.72, 95% CI 0.53-0.98, p = 0.0355), but not overall DR and proliferative DR. Overall, this study demonstrated through a population-based cohort analysis and a Mendelian randomization analysis that GLP-1 RAs are associated with decreased risk of developing DR.
Clinical outcomes of pediatric osteomyelitis
1. Pediatric patients under 18 years with chronic osteomyelitis were more likely to have long-term orthopedic follow-up, pathologic fractures, and require multiple surgeries, compared to patients with acute osteomyelitis.
2. There were no differences in rates of limb length discrepancies, readmission rates, or fatality, between acute and chronic osteomyelitis pediatric patients.
3. Limb length discrepancies, pathologic fractures, and fatality were rare sequelae amongst all pediatric osteomyelitis patients.
Evidence Rating Level: 2 (Good)
Complications of osteomyelitis in children may include limb length discrepancies and pathologic fractures. However, there is a lack of data on long-term clinical complications, particularly data from multi-centre studies. Therefore, this current retrospective cohort based in the United States examined the clinical outcomes of pediatric osteomyelitis, both acute and chronic, hypothesizing that chronic osteomyelitis would result in longer hospital stays and increased rates of limb length discrepancies and pathologic fractures. The study population consisted of children under 18 years diagnosed with osteomyelitis in 2015 (excluding patients with septic arthritis alone) taken from the HealthFacts database, which includes hospitals across the United States using the Cerner medical record platform. Sequelae were assessed for within 2 years after diagnosis. In total, there were 869 patients included, with acute osteomyelitis comprising 60.5% of cases. The study found that both acute and chronic osteomyelitis occurred most commonly in the winter, and more often in the Midwest and South than the Northeast or West (p = 0.03). Children with chronic osteomyelitis were older (12.0 years vs 9.5 years, p = 0.0004). As well, chronic osteomyelitis was more often associated with long-term orthopedic follow-up (14.0% vs 4.8%, p < 0.0001). In terms of sequelae, fatality was rare and not significantly different in chronic or acute osteomyelitis, with 2 deaths in each group (0.5% and 0.3% respectively). Limb length discrepancies were also infrequent and comparable between both chronic and acute (1.2% versus 1.3%, p = 0.83). Readmission rates were also not significantly different between chronic and acute (5.8% versus 6.7%, p = 0.31). Though also rare, pathologic fractures occurred more often in chronic than acute osteomyelitis (p = 0.003), and chronic osteomyelitis was associated more with multiple surgeries (46.0% versus 29.3%, p = 0.04). Overall, this study demonstrated that severe complications from acute or chronic osteomyelitis are rare, though chronic osteomyelitis is associated with a higher risk of pathologic fractures, requiring multiple surgeries, and long-term orthopedic follow-up.
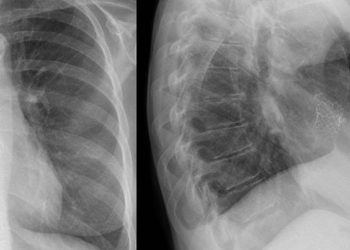
1. For patients with idiopathic pulmonary fibrosis (IPF), there was no difference in pulmonary function and efficacy between patients on low-dose pirfenidone compared to standard dose.
2. Patients on low-dose pirfenidone were more likely to be older than those on standard dose, and were also more likely to report experiencing gastrointestinal and skin side effects.
Evidence Rating Level: 2 (Good)
Idiopathic pulmonary fibrosis (IPF) is a progressive interstitial lung disease with a median survival of 3-5 years. While the antifibrotic drug pirfenidone is known to decrease decline of lung function in IPF patients, it is also associated with adverse gastrointestinal and skin-related events. Although some studies suggest low-dose pirfenidone is non-inferior to standard dosing, the burden of adverse side effects in low-dose pirfenidone is not well-known. Therefore, this single-centre study based in South Korea aimed to elucidate the factors associated with pirfenidone dose reduction. The study population consisted of IPF patients treated with pirfenidone, with 1 or more follow-up visits that assessed for adverse side effects. In this study, a standard dose was considered 1800 mg/day, whereas low-dose was less than 1800 mg/day. In total, there were 156 patients included, with a mean age of 69.7 years, and a median (IQR) follow-up of 243 (84-385) days. The study found that those taking low-dose pirfenidone were more likely older (71.0 years vs 67.4 years, p = 0.016), less likely to be ever-smokers (80.8% vs 96.4%, p = 0.008), and more likely to have a lower BMI (24.1 kg/m2 vs 25.7 kg/m2, p = 0.027). There were no differences in pulmonary fit test results, exercise capacity, or rates of pulmonary hypertension between the standard and low-dose groups, though more patients on standard dosing had emphysema (p = 0.048). After adjusting for sex, BMI, smoking status, and emphysema, older age was associated with reduction of pirfenidone dose (OR 1.066, p = 0.016). In addition, there were higher rates of some adverse events reported in the low-dose compared to the standard dose group, including anorexia (20.5% vs 3.5%, p = 0.004), urticaria (24.7% vs 10.5%, p = 0.039), and generalized weakness (9.6% vs 0.0%, p = 0.018). More broadly, the low-dose group experienced higher rates of gastrointestinal side effects (p < 0.01) and skin side effects (p = 0.020) than the standard group. Overall, this study demonstrated that older patients were more likely to be on low-dose pirfenidone, and that individuals in the low-dose group were more likely to experience side effects, though there were no differences in pulmonary function and efficacy of pirfenidone between the groups.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.