2 Minute Medicine Rewind June 22, 2020
1. PPI use may be associated with an increased mortality risk in patients who have received kidney transplants.
Evidence Rating Level: 1 (Excellent)
Proton-pump inhibitors (PPIs) are commonly prescribed to kidney transplant recipients (KTRs) to protect against gastrointestinal symptoms and complications induced by their immunosuppressive therapy. Although PPIs are generally well-tolerated, numerous observational studies have demonstrated that chronic PPI use is associated with adverse health outcomes, such as increased nutritional deficiencies. A post hoc analysis of the TransplantLines Food and Nutrition Biobank and Cohort Study, a longitudinal study of American veterans (n= 349 312, median followup= 8.2years), found an increased mortality risk in PPI users compared to nonusers (n=703 KTRs, HR 1.86, P<0.001). This association remained independent after adjusting for potential confounding variables, such as medication use and comorbidities (HR 1.68, P=0.002). Specifically, PPI use was associated with an increased risk of mortality from cardiovascular causes (HR 2.42, P<0.001). Subgroup analyses also showed that this association appears to be dose dependent, with premature mortality highest in KTRs taking more than 20mg omeprazole equivalents/day (Ptrend<0.001). The results of their replication study, using an independent cohort of stable KTRS from University Hospitals Leuven (n=329, median followup= 3.7 years), showed similar results to those in the TransplantLines study. Prospective analyses showed PPI users had over twice the mortality risk of nonusers (HR 2.47, P<0.001), which remained significant after adjusting for potential confounders (HR 1.75, P=0.01). Further research is needed to fully elucidate whether there is a a cause-effect relationship between PPI use and its association with increased mortality risk in KTRs (i.e. conducting an RCT), and if it exists, by what mechanism.
Effects of a modestly lower carbohydrate diet in gestational diabetes: a randomized controlled trial
1. A modestly lower carbohydrate diet neither increased ketonemia nor improved glycemic control in pregnant women
Evidence Rating Level: 2 (Good)
Although meta-analyses have shown significant improvements in HbA1c and greater weight loss with low-carbohydrate diets in the context of type 2 diabetes and obesity, there is a lack of consensus on the most effective diet for gestational diabetes (GDM). GDM is rising in prevalence and associated with adverse pregnancy outcomes, such as macrosomia and cesarean section. However, low-carbohydrate diets in pregnancy may increase maternal ketone concentrations, which have been associated inversely with offspring intelligence, even without ketoacidosis. Therefore, a modestly lower carbohydrate diet (MLC) was hypothesized to lower glucose levels without inducing ketonemia. MAMI I (Macronutrient Adjustments in Mother wIth gestational diabetes study I) was a six week, two-arm, parallel RCT conducted on pregnant women between 18-45 years old with a GDM diagnosis at 24-32 weeks of gestation. 46 patients were randomly allocated (stratified by age and BMI) to either a diet of 135g of carbohydrates/day or routine care, targeting 180-200g/day (RC), with allocation of treatment concealed from the dietician. Through a modified ITT analysis, no detectable differences in blood ketone concentrations (BHB) between the dietary groups were found (MLC 0.1+0.0, RC 0.1 +0.0, P=0.34). According to their food diaries at the end of the trial, only 20% of the women in the intervention group met the carbohydrate target, while 66% of all participants had already developed some carbohydrate restriction at baseline. The intervention group had significantly lower dietary intakes of iron and iodine, with only a third of the women in the intervention group meeting nutrient reference values (MLC 32% vs RC 67% for iron, MLC 39% vs 89% for iodine). No differences were found in secondary outcomes, in weight or gestational age at delivery, fat mass, macrosomia, or large-for-gestational age infants. There was no difference in glycemia (MLC 6.1+ 0.1, RC 6.0+0.1mmol/L), nor was ketonemia found to be affected by exogenous insulin use (P=0.97). Though small changes in ketonuria are not considered clinically important, the final sample size had 77% power to detect a 0.04 mmol/L difference in BHB. More appropriately powered studies with larger sample sizes and food provision to increase dietary compliance are necessary to assess the benefits and risks associated with a modestly lower carbohydrate diet in GDM.
1. Hookworms was found to be a safe and well tolerated treatment option possibly associated with an immunobiological effect in relapsing multiple sclerosis.
Evidence Rating Level: 2 (Good)
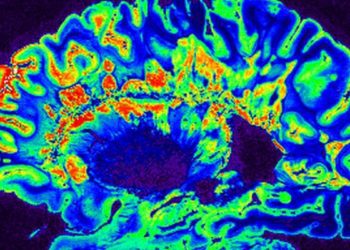
Multiple sclerosis (MS), an immune-mediated central nervous system disease, is associated with an imbalance between inflammatory cytokines and immunoregulatory factors, namely regulatory T cells (Tregs). Compared to matched uninfected MS controls over 5 years, MS patients naturally infected with gastrointestinal parasites have milder disease, which is associated with higher Treg activity. Some small, non-placebo-controlled, short duration studies have found patients infected with N americanus larvae to have favourable MRI and immunological outcomes in their autoimmune and allergic conditions. In this 9 month, double-blind, placebo-controlled trial, 71 patients were randomized in a 1:1 ratio to receive either experimental infection with 25 N americanus L3 larvae (HW treatment) or placebo (pharmacopoeial-grade water). At baseline, there was no difference between the groups in T2 lesion load and there was a higher percentage of T cells in the placebo than the HW arm. At nine months, there was no significant difference in new, enlarging, or enhancing brain lesions between the groups (154 in HW, 164 in placebo) at 9 months, while there was a higher number of scans without detectable MRI activity in the treatment group (51% vs 28% placebo). There was an increase in Tregs in the HW arm and a decrease in the placebo group, without reaching significance, and four patients in the HW arm compared to 10 in placebo experienced relapses during the trial. No patients withdrew because of adverse effects from the HW infection and there were no differences in adverse effects between groups next to initial skin discomfort when the worms were applied to the arm (82% vs 28%). This trial showed that treatment with hookworm was safe and well-tolerated, with the increased Treg count suggesting a possible immunobiological effect despite no difference in the primary outcome of lesions between groups. Further study with a design and sample powered to compare the proportion of patients without disease activity and a longer treatment duration (1-2 years) would be needed to assess clinical response, but preliminary findings are promising for a potential new therapeutic option in the future.
Cholesterol Metabolism by Uncultured Human Gut Bacteria Influences Host Cholesterol Level
1. Gut Bacterial Species Shown to Lower Fecal and Serum Cholesterol Levels in Humans
Evidence Rating Level: 2 (Good)
High serum cholesterol levels have been linked to cardiovascular disease, the cause of 1 in 4 deaths in all industrialized countries. Reducing cholesterol transport in the intestine, as demonstrated by ezetimibe, a small molecule transporter inhibitor, is a clinically validated strategy to lower cholesterol serum levels. Past studies have shown that the presence of certain gut bacteria are similarly linked to lowering serum and fecal cholesterol levels. A proposed mechanism involves the bacteria converting cholesterol to coprostanol, thereby decreasing the amount of absorbed cholesterol. However, support for this mechanism is lacking in the current literature. Through a bioinformatics analysis, the study identified 4 clusters of enzymes from the human gut microbiota with the potential to metabolize cholesterol. These enzymes were then experimentally validated as cholesterol dehydrogenases, out of which the ECOP170 enzyme was identified as having the greatest expression increase in the presence of cholesterol. Subsequently, the ECOP170 genes were renamed as ismA (intestinal metabolism sterol A genes). A subsequent in-vivo analysis was conducted on two independent human cohorts, PRISM and HMP2, separating coprostanol positive fecal samples from coprostanol negative samples within those cohorts. The analysis found that the presence of IsmA-encoding bacteria in the gut was highly correlated with the presence of coprostanol in feces, suggesting that these bacteria metabolize cholesterol in-vivo (PRISM: OR = 42.73 [95% confidence interval, CI: 11.28, 283.54]; HMP2: OR = 28.94 [95% CI: 13.64, 61.41]). Finally, a meta-analysis of 3 studies found that the presence of IsmA-encoding bacteria was highly correlated with a decrease in serum cholesterol levels. The human cohort with IsmA-encoding bacteria had a 0.15 mmol/L lower total serum cholesterol level, compared to a cohort without IsmA-encoding bacteria (95% CI: −0.27, −0.03). This effect size is comparable to differences in cholesterol levels due to human gene variation: For instance, HMGCR and PCKS9 are lipid-associated genes that have been found to contribute differences in cholesterol levels of 0.063 mmol/L and 0.050 mmol/L respectively. This suggests that the presence of IsmA-encoding bacteria contributes a biologically significant decrease in host serum cholesterol levels, which could directly impact human health outcomes. This multidisciplinary strategy in combining bioinformatic and biochemical approaches could be applied to other pathways and microbiomes of interest to characterize previously unknown microbes and enzymes that could be responsible for other relevant metabolic transformations.
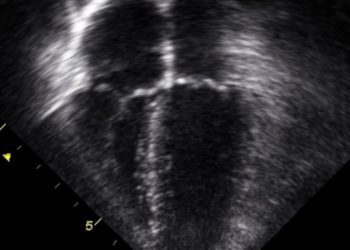
1. Heart failure patients whose EF deteriorated from ≥50% to between 40% and 50% were at an increased risk of mortality and cardiovascular events
Evidence Level Rating: 2 (Good)
Clinicians use left ventricular ejection fraction (LVEF) to guide treatment of heart failure (HF). Patients with HF are commonly divided into two separate and clinically distinct cohorts, those with an EF <40% having “heart failure with reduced ejection fraction” (HFrEF) and those with an EF ≥50% having “heart failure with persevered ejection fraction” (HFpEF). This categorization, however, fails to account for patients with an EF between 40% and 50%, sometimes classified as having “heart failure with mid-range ejection fraction” (HFmrEF). The aim of this study was to determine future risk of cardiovascular events based on a prior transition into the HFmrEF group, either by reduction or increase in EF from a previous measurement. Primary outcomes included all-cause mortality, cardiovascular mortality, and all-cause hospitalization, among others. Using health records from the UC San Diego Health System, 448 patients with HFmrEF were identified and followed over an additional two years to track outcomes. 157 patients (M [SD] age = 63.8 [8.1] years, 63.7% male, 54.7% white) improved, 67 patients (M [SD] age = 66.6 [9.8] years, 75.0% male, 64.0% white) remained stable, and 224 patients (M [SD] age = 70.9 [9.5] years, 56.3% male, 62.5% white) deteriorated with regards to their EF prior to inclusion. A 1.34-fold increase in the risk of combined all-cause mortality and hospitalization was seen in the deteriorated group (p = 0.03). The deteriorated group was also at a significantly increased risk of cardiovascular death or hospitalization for HF (HR 1.71, 95% CI 1.08 to 2.50, p = 0.02). Both findings were consistent after adjusting for age, sex, and comorbidity. In contrast, there was no significant difference in risk for any of the primary outcomes between patients in the improved and stable groups even after adjustment. Overall, this study suggests that the directional change of EF in HFmrEF patients has implications for future clinical course and could be used to guide and tailor therapy.
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.